Clinical use cases
Multiple sclerosis
The DIFUTURE consortium’s doctors and scientists are active in multiple sclerosis (MS) research. The scope of data that have already been integrated is broad, ranging from clinical and laboratory data, to multi-dimensional images, to genetic information. Furthermore, there are extensive, largely standardised data collections available. Distributed analyses will be conducted with the aim, in particular, of identifying markers and algorithms to predict disease progression – and to allow targeted, personalised treatment from an early stage.
Parkinson’s disease
For the Parkinson’s disease (PD) use case, the DIFUTURE consortium will build upon the integration and analysis methods employed for the MS use case. The PD project, too, will entail the harmonisation of diverse types of data – and their integration in conjunction with robust quality control, making them available for analysis. This use case and others – including for rare illnesses, cancer, stroke, and cardiovascular disease – are aimed at enabling precision medicine. The goal is to significantly improve treatment, (early) diagnosis, prevention and aftercare.
Oncology
In the oncology use case, the HiGHmed consortium will address the challenges associated with incorporating huge data volumes from genome sequencing (omics data) and radiology into clinical practice. A virtual oncology centre will visualise cancer treatment, and serve as a platform for sharing information between hospitals, research institutions, doctors and patients. The virtual centre will play a significant role in identifying cancer cases of similar kinds, and enabling tailored, patient-centred care – as demonstrated by examples involving tumours of the pancreas, liver and bile ducts.
Cardiology
In the cardiology use case, the HiGHmed consortium will import data from wearable, implanted or connected medical devices to the IT architecture of the data integration centres. New, mobile diagnostic devices will have a major impact on medical practice and research. They capture data from long-term monitoring and measurements, generating highly specific and comprehensive data sets. As a result, high-risk patients could be identified early, hospital stays reduced, and mortality rates lowered.
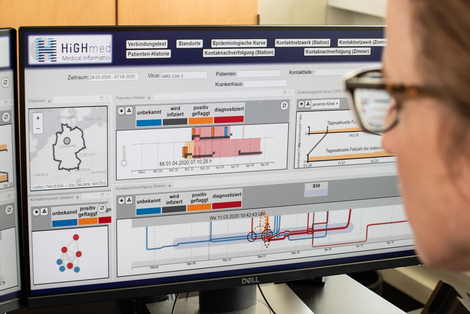
Infection control
In its infection control use case, the HiGHmed consortium will develop an automated early-warning and cluster-analysis system to support the algorithmic detection of pathogen clusters in hospitals. This includes the identification of multidrug-resistant pathogen clusters, and their transmission routes within and between hospitals. It will also help determine whether clusters represent genuine outbreaks, and identify potential causes of outbreaks and transmission.
ASIC - Algorithmic Surveillance in Intensive Care
With the ASIC use case, the SMITH consortium promotes the improvement of patient care by using already existing clinical routine data. This will be shown using the example of the therapy of patients with acute lung failure (ARDS), a disease from which about 40 percent of all affected patients still die today. The ASIC app developed for this purpose functions as an early warning system by alerting doctors to potential ARDS before the patient's condition threatens to become critical.
HELP - Guideline-based Use of Antibiotics in Infectious Medicine
With the HELP use case, the SMITH consortium focuses on the guideline-based and recommended use of antibiotics for early and targeted control of certain bacterial infections. The main focus lies on the support of infectiology in normal and intensive care units using the HELP app developed for this purpose. This provides medical staff with rapid information and recommendations for responsible antibiotic therapy in staphylococcal bloodstream infections.
Infrastructural and methodological use cases
Patient recruitment for clinical studies
Many clinical studies fall at the first hurdle because they lack a sufficient number of participants. To improve the recruitment process using IT and available routine data, the MIRACUM consortium will – in the use case “Alerting in care – IT support for patient recruitment” – integrate corresponding platforms into the healthcare information system (HIS) infrastructure at each of its university hospitals. Regular evaluation and feedback loops will help continuously improve the quality of documentation and ensure the completeness of data elements used for recruitment.
Predictive models for clinical decision-making
The gradual expansion of MII data integration centres lays the foundations for identifying and stratifying patient cohorts into subgroups based on clinical parameters, biomarkers and molecular/genomic data – with the goal of developing subgroup-specific predictive models. In the use case “From data to knowledge – clinico-molecular predictive knowledge tool”, the MIRACUM consortium will integrate smart, FHIR-based apps into healthcare information system (HIS) environments. This will help put these predictive models into practice, and support doctors with diagnostics and treatment decision-making. The initial clinical focus will be on lung diseases and brain tumours.
Data visualisation for the support of treatment decision-making
In the context of tumours, precision medicine is already very advanced. Many tumours can now be identified by driver mutations, and therefore treated in a targeted way. Moreover, clinical information, images, and molecular/genetic test results are combined and shared via molecular tumour boards (MTB) to aid interdisciplinary decision-making. In this context, the MIRACUM consortium will develop innovative IT solutions to improve the complex processes associated with quality assurance, data processing, data integration and information research that take place between high-throughput genetic analyses and treatment decision-making. Additionally, hospitals will benefit from efficient data-visualisation tools that help them choose the right therapies.
PheP – Phenotyping pipeline supporting clinical evaluation projects
In the methodological use case Phenotyping Pipeline, PheP for short, SMITH develops innovative data analytical methods that automatically extract medical information from electronic patient records. Evaluation projects and calculations on existing data lead to ever new patient-related information and to a differentiated characterization of human attributes, so-called phenotypes. The rich data pool enables long-term optimization of clinical research and patient care.