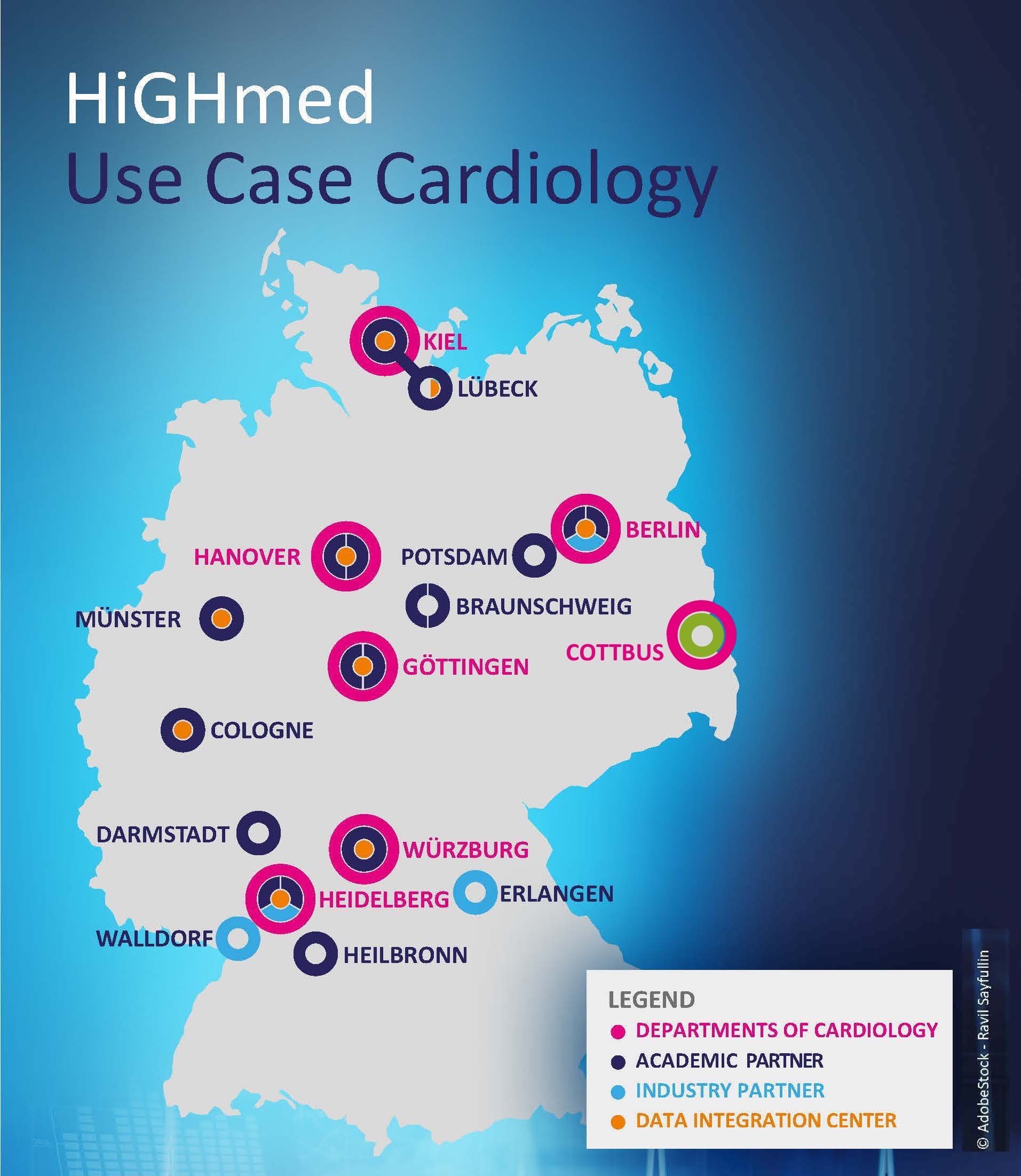
In the cardiology use case of the HiGHmed consortium, clinicians, medical informatics specialists and data scientists from six university hospitals (Berlin, Göttingen, Hannover, Heidelberg, Kiel and Würzburg) and numerous partners from science, industry and healthcare work hand in hand. Their common goal is to improve the long-term health care of patients with chronic heart failure through the use of medical informatics technologies.
In order to achieve this, the health data of patients with chronic heart failure at the participating HiGHmed sites are described in a uniform manner, compiled in so-called data integration centers at the university medical sites and made available for cross-site evaluations of research.
HiGHmed makes medical data collected in routine care usable for research. Disease-related information - routinely collected during a hospital stay - is documented, coded and stored in a uniform manner and then evaluated across sites in compliance with all current data protection regulations and in accordance with the patient's declaration of consent. The aim is to identify high-risk patients and signs of deterioration in their condition at an earlier stage and to develop approaches for more individualized treatment.
Standardized data and data models play a central role here. They first enable uniform documentation in the respective clinics and then enable data exchange for joint analysis. All sites involved in the use case have agreed on uniform data models as a basis for the exchange and preparation of data for research. They use as a basis the data model of the German Center for Cardiovascular Research e.V. (DZHK). This allows data from more than 20 clinical trials with over 7,000 patients and other DZHK-associated studies to be compared directly with the treatment data provided as part of the cardiology use case. In addition, all sites have reconciled a dataset that extends the DZHK base dataset with the most relevant data for chronic heart failure.
For research, the development of patients after leaving the hospital is currently still a blind spot. In order to also collect data from patients' everyday lives and thus be able to take into account information outside the hospital stay in the analyses, the use case partners are testing the use of portable sensors and apps, so-called wearables.
In spring/summer 2021, the first patients will be equipped with smartwatches and smartphones to record activity parameters and heart rate data, for example. By analyzing this data, it should be possible in the long term to detect deterioration episodes at an early stage in patients with a high risk of severe disease progression, to improve their quality of life and to reduce hospital stays. In the future, the results of the cardiology use case will enable patients to bring together all relevant aspects of their individual disease course and make them available for their treatment and medical research. The use case can also provide insights for research into other disease patterns that, like heart failure, exhibit an episodic deterioration in health, such as multiple sclerosis or chronic obstructive pulmonary disease.
"In the cardiology use case, we pursue the goal of sustainably improving the care options and quality of life of patients - over 3 million in Germany alone - with often chronic heart failure. To achieve this, it is enormously important to have fast and structured access to all relevant information about a patient. In emergency situations in particular, this can even save lives.
It is not enough to merely collect the data. With the help of state-of-the-art technologies, we create new and sustainable structures through which the care data can be actively used. Future patients can benefit directly from this by receiving more individualized care and by therapies being continuously optimized based on new findings. Innovative data structures form the basis for scientific analyses of the care data, which then enable these new findings and individualized treatment for each patient."
Prof. Udo Bavendiek
Chief Physician, Clinic for Cardiology and Angiology, Medical University Hannover
Information box: |
Since 2018 patients of the use case cardiology have been recruited for a pilot study.
The podcast episode "Medical Data for a Better Life with Heart Failure - The Cardiology Use Case", which matches the topic can be found here.
The article associated with our use case, "Chronic heart failure: wearable sensors and apps to improve research and care," can be read here. |